The biological gear required to bear offspring is one of the scientific hallmarks of being a female. Not all women have all that gear, but men don’t have any of it. This is a scientific fact that applies to all mammals except for that extremely rare hermaphrodite who has both male and female sexual traits.
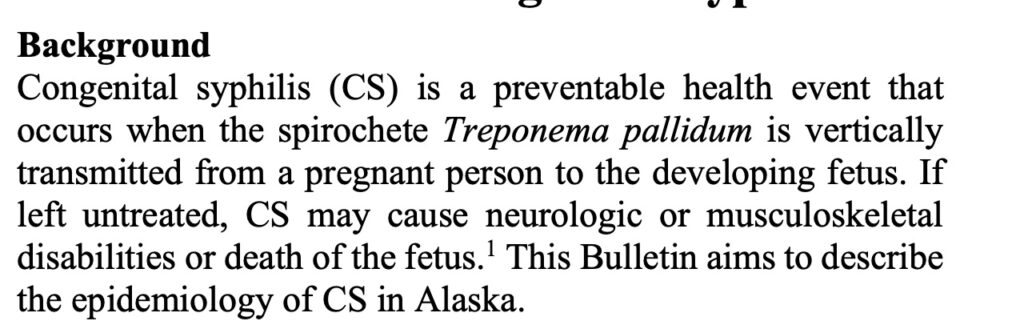
But in the most recent report on congenital (born with) syphilis in Alaska, the Alaska Department of Health has decided that women who are pregnant are now known by the politically correct term, “pregnant people.”
Pregnant people a phrase that is now commonly in use among scientists at the Centers for Disease Control and Prevention, as the medical profession turns away from science and biology and adopts an attitude that gender is something that is “assigned at birth,” rather than observed at birth (or in utero), and that men can become pregnant.
As for the baby boys and girls born with syphilis in Alaska, they came into the world with a condition that can be fatal if left untreated.
The current uptick in syphilis in Alaska was detected in 2018, and seems to have been exacerbated by the Covid-10 pandemic policies. The same trend has been observed nationally.
During 2018–2022, 26 congenital syphilis cases were identified in Alaska, one of them being fatal.
In Alaska, most cases have occurred in people who self-identify as heterosexual and are living in urban environments, with 29% of the people diagnosed with syphilis having been identified as either experiencing homelessness or a great deal of housing instability in 2021. Most (69%) of the infected mothers reported heroin, amphetamine, methamphetamine, or cocaine use within 12 months of the case investigation.
All mothers giving birth to babies with congenital syphilis were between 16 and 37 years. Some 85% were Anchorage residents and 58% were identified as Alaska Native/American Indian only on the infant’s birth certificate. Sixty-five percent of the mothers had the equivalent of a high school diploma or more education. Addiction and drug use is a big factor among these women, the State report says.
Yet the report is confused on the matter of gender and sex. In one instance, the Health Department talks about mothers. But then, when the syphilis report talks about fetuses and pregnancy, the scientists switch and refer to moms-to-be as “pregnant people.” It is tiptoeing around the gender ideology debate by avoiding gender altogether at times, while at other times, it can’t seem to avoid the word “mother.”
“While no inherent aspects of a mother’s race or education create risk, the disparate social conditions surrounding these factors, such as housing instability and substance use, can be contributing risk factors. Third, further investigation of these CS cases, such as through a multi- disciplinary review committee, should examine the factors and conditions that impact access to adequate prenatal care to ensure early syphilis detection among pregnant persons.“
CDC data indicate that the rate of primary and secondary syphilis among American Indian and Alaska Natives in 2021 was 42.2 per 100,000, nearly five times that of white individuals, up 520 percent from 8.0 per 100,000 among American Indian/Alaska Natives in 2016. In the same time period, congenital syphilis has increased over 900 percent among this group (rate of 37.7 per 100,000 live births in 2016 compared to 363.7 in 2021) and is almost 10 times higher than among whites.
The Health Department recommends that medical providers:
- “Screen all pregnant people (regardless of risk factors) during their first prenatal visit, during their third trimester of pregnancy, and at the time of delivery.
- “Screen pregnant people seen for medical services unrelated to their pregnancy (e.g., during an outpatient clinic, urgent care, or emergency department visit) if they have not already had prenatal care with appropriate syphilis screening or if they are at increased risk for syphilis acquisition (e.g., sex with multiple partners, sex in conjunction with drug use or transactional sex, late entry to prenatal care or no prenatal care, methamphetamine or heroin use, incarceration of the pregnant person or their partner, and unstable housing or homelessness).
- “Diagnostic considerations for pregnant people are available on CDC’s Syphilis During Pregnancy website.
The full report on congenital syphilis can be found at this link.
As for treatment, the State Health Department notes that there is a shortage of the type of penicillin needed to cure this disease:
- “The FDA listed a shortage of penicillin G benzathine injectable suspension products (Bicillin L-A®) on April 26, 2023. Pfizer provided an availability update on June 12, 2023, with an expected recovery in the second quarter of 2024. There are no emergency stockpiles of this medication, and product is being allocated with limited inventory released, resulting in the supply not meeting demand.
- “Bicillin L-A® is the only CDC-recommended treatment for some patients, including pregnant people infected with or exposed to syphilis, and babies with congenital syphilis. Although Bicillin L-A® remains the treatment of choice for patients with syphilis, CDC has recommended that healthcare providers prioritize the use of Bicillin L-A® to treat pregnant people and babies with congenital syphilis. ®
- “Consider prioritizing unstably housed/homeless persons for Bicillin L-A treatment after pregnant people infected with or exposed to syphilis and babies with congenital syphilis.
- “Doxycycline is an alternative therapy for non-pregnant patients diagnosed with or exposed to syphilis; however, doxycycline is an FDA Pregnancy Category D medication, and is not recommended as an alternative treatment for pregnant individuals.”
The National Institutes of Health considers “pregnant people” to be an inclusive and acceptable phrase for the medical community when referring to women who are pregnant but who are masquerading as men through transgender medical treatment.